
The brain-gut connection: how TCM has known for centuries what Western medicine is now discovering
- Recent research has found that bacteria in the gut can affect people’s mental state, leading to mood, cognition and behavioural problems
- But in traditional Chinese medicine, the link between the gut and all of the body’s organs has been recognised for thousands of years
Trusting your gut may be good advice, but it hardly qualifies as medical science. Or does it?
Research increasingly shows that the connection between our “gut” and our brains – especially our emotions and mental health – is closer than has ever been imagined. In recent headlines and medical research papers, doctors and researchers are employing a new term for the gut: the second brain.
Research such as that from doctors Braden Kuo and Allan Goldstein at Massachusetts General Hospital, the US, who found that bacteria in the gut can affect mood, cognition and behaviour is increasingly exciting to fellow doctors and scientists.
But practitioners of traditional Chinese medicine (TCM) can be left exasperated. They say that Chinese medicine has understood the connection between the gut and the body’s overall health for thousands of years.

“When I see patients, the first thing I do is to assess their gut health,” says Ronald Hubbs, a licensed acupuncturist and professional herbalist in Portland in the US state of Oregon. And while recent research into the mind-gut connection is getting press, Hubbs says that “the vast majority of mainstream Western doctors and health-care practitioners are still treating the mind as something separate from the rest of the body. And many patients are continuing to suffer.”
Western medicine and TCM are often thought to be at odds. TCM believers and practitioners routinely feel underserved and derided by Western medicine. Western doctors in many cases dismiss TCM’s conception of the body, the basic framework of its treatments and its lack of reliance on the scientific method.

But despite all their differences, when it comes to the mind-gut connection, these two disparate modes of treating the body have come to surprisingly similar conclusions: our hearts may pump our blood, but in many cases, our feelings originate in our gut.
Jay Pasricha, director of the Johns Hopkins Centre for Neurogastroenterology, offers the following example of our new way of conceptualising the gut-brain connection on the Johns Hopkins website. While doctors have always known that mental conditions such as stress and anxiety can lead to gastrointestinal issues – butterflies in your stomach for example, or stress-induced loose stools or nausea – increasingly it seems that the cause-and-effect relationship between mental state and gastrointestinal state may work in reverse, as well.
An upset gut can trigger changes in our mental state, suggesting that an upset in the balance of gastrointestinal function could conversely be sending signals to your brain that cause neurological and emotional symptoms such as depression, anxiety and mood swings.
While modern Western medicine has brilliantly discovered many of the material aspects of health science, it is just now starting to realise how much the mind and emotions are affected by the gut
What is the “gut” exactly? In Western medicine, the gut refers to the entire gastrointestinal system, the tract from your where food is swallowed to where waste is eliminated – from oesophagus to rectum.
The Chinese traditional conception of the gut is slightly different. “Traditional Chinese medicine refers to the gut as the spleen and stomach,” says Peter Yeung, an acupuncturist and Chinese medicine practitioner with a practice in Los Angeles.
It can be difficult to understand how digestion can be linked to the brain and how your gut can influence your emotions, thoughts and even how you make decisions.
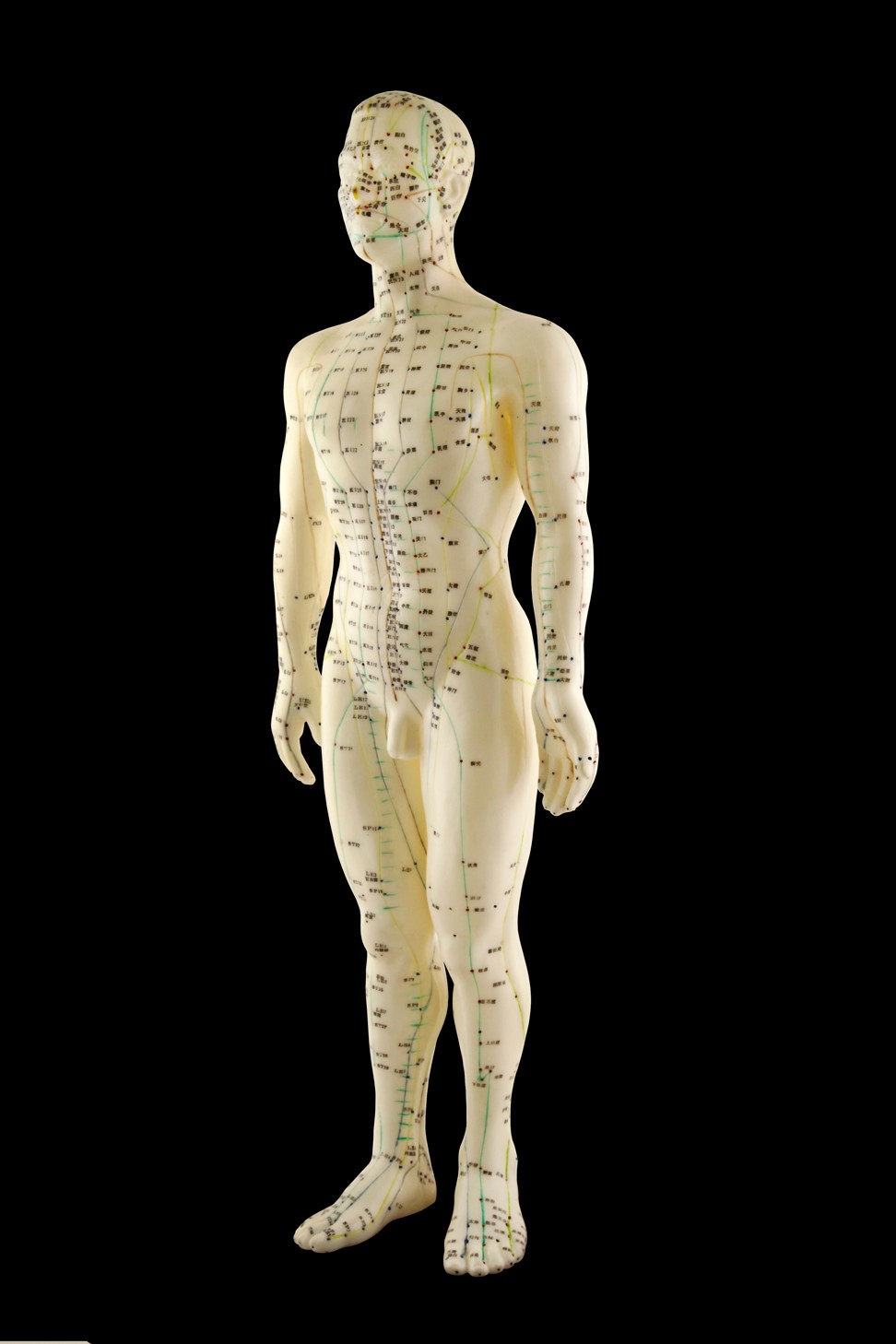
“In TCM, we don’t view the body as each separate part,” Yeung says. “We see it as a whole. There are 12 main energy channels, called meridians, in the human body. They run through the entire body, from the top to the bottom.
“For example, in acupuncture we can needle areas in the feet to treat neck pain. We can needle the leg to treat digestive disorders. There are points on the hand that treat headaches, lower back pain, sciatica. Our ancestors were very smart and the maps of the energy channels in the whole body were mapped out thousands of years ago.”

Western medicine does not put much credence in the idea of meridians, but it does embrace the interconnectedness of the body – in the most obvious case via the nervous system. Now, doctors and researchers are increasingly highlighting the role of the enteric nervous system, the network of more than 100 million nerve cells lining the entire gastrointestinal system.
Doctors may refer to the gut as the second brain, but that does not mean that the gut on its own is capable of thought. Instead, the nerves in the gut act as a vital conduit of information to the brain; the gut and the brain are in constant communication.
This new understanding opens up a new world of treatment options for both mental health and gastrointestinal issues. If the mind and the gut are so intimately connected, then a doctor could potentially address gut problems by treating mental health, and vice versa – for example, see recent successes treating irritable bowel syndrome with antidepressants or cognitive behavioural therapy.
If Western doctors are excited by these new findings, TCM practitioners are mostly bemused.
“In Chinese medicine, the connection between the gut and all of the organs has always been recognised,” says Hubbs.
“While modern Western medicine has brilliantly discovered many of the material aspects of health science, it is just now starting to realise how much the mind and emotions are affected by the gut. Once scoffed at, Chinese theories are now being proved by modern medicine.”

Take small intestinal bacterial overgrowth (SIBO), a recognised medical condition in which the sufferer has an abnormally large population of bacteria in their small intestine which can lead to many gastrointestinal symptoms such as diarrhoea, constipation, abdominal pain, and nausea.
The traditional Chinese diagnosis for the same condition is known as Gu, and while Gu has the same gastrointestinal symptoms as SIBO, TCM texts also say that Gu can cause symptoms that “resemble mental illness”, according to Hubbs, “including depression, fits of anger or rage, muddled thinking, restlessness, and mental exhaustion”.
While cognitive symptoms presenting for a gastrointestinal condition would have been dismissed outright not long ago, these days the idea that your stomach ache and your emotional outlook are connected should give neurological and gastrointestinal researchers pause.
According to both cutting-edge research and ancient Chinese texts, they would do well to listen to their guts.

